
A comparison of scalpel-bougie-tube and Cric-Guide® in a simulated obese bleeding tissue model
Highlight box
Key findings
• In the simulated obese bleeding neck, Cric-Guide® facilitates faster intubation of the trachea in emergency front of neck access at the expense of greater posterior tracheal wall damage.
What is known and what is new?
• Cric-Guide® has previously been shown to perform as well as scalpel-bougie-tube in the simulated obese neck or the slim bleeding neck.
• This manuscript adds data on Cric-Guides® performance in the simulated obese and bleeding neck.
What is the implication, and what should change now?
• Further work is needed to study whether a shorter device would remain faster, but reduce the incidence and degree of posterior laryngeal wall trauma.
Introduction
Difficult Airway Society (DAS) guidelines for the management of unanticipated difficult intubation (1) recommend the scalpel-bougie-tube (SBT) technique. It entails using an 8–10 cm vertical incision in the midline of the neck for emergency front of neck access (eFONA) in patients with obesity or impalpable landmarks.
Performing eFONA in the obese patient is challenging. Excessive subcutaneous adipose tissue necessitates deeper surgical dissection and increases the risk of bleeding. Blood in the surgical field can obscure the cricothyroid membrane (CTM) leading to false passage creation and difficult endotracheal tube (ETT) insertion (2).
A novel cricothyroidotomy introducer, the Cric-Guide® (Figure 1), has been developed in order to facilitate eFONA. It has a sharp, 8 mm wide leading edge, that acts as a scalpel, with a 6mm wide guiding channel to allow smooth passage of the bougie into the trachea. Three sizes of Cric-Guide® have been designed to be selected based on the patient’s body weight (see Appendix 1). A previous study using this instrument demonstrated successful eFONA in a simulated obese porcine laryngeal model (3).
We hypothesised that the Cric-Guide® performed better than the SBT technique for eFONA in an obese bleeding model. Our primary objective was to compare the time taken to secure the airway using the Cric-Guide® compared to the SBT technique in an ex-vivo pig neck tissue model designed to simulate eFONA in the difficult to access, bleeding neck.
Methods
The study protocol was reviewed by the Clinical Governance Department of Tayside Health Board and deemed not to require ethical review (on April 21, project registration number 017/21). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All participants gave their consent to participate in the study. The study consisted of 3 phases: development of a porcine model; training anaesthetists on the use of the Cric-Guide® and the SBT technique; and testing performance. The study was carried out between March and October 2021.
Porcine model
We created a model that simulated the external airway anatomy of an obese patient. The model consisted of a porcine larynx with attached trachea and overlaid with pork belly purchased from a medical meat supplier (MedMeat Ltd., Oldham, UK). We ensured that the pork belly was between 15–20 mm thick to correlate with previously published work on depth to the CTM in severely obese [body mass index (BMI) >45 kg/m2] individuals (4). This was mounted in a larynx holder designed for use with an animal larynx (MedMeat Ltd., Oldham, UK).
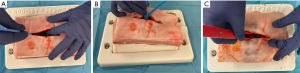
In order to replicate bleeding associated with eFONA in an obese patient, we infiltrated 30 mL of stage blood—used to simulate blood in film and theatre productions. Figure 2 demonstrates the degree of bleeding produced when model was incised and techniques performed.
Training
We invited consultant anaesthetists and senior trainees [speciality trainee (ST) year 6/7] from the anaesthetic department of Ninewells Hospital, Dundee who have undertaken instruction in eFONA as part of core airway skills training. Prior to the study, we collected data on participants who had clinical experience of eFONA. Participants were given an information leaflet describing the use of the Cric-Guide® introducer (5,6) for emergency airway access and the SBT technique, then shown an instructional video. Thereafter, participants repeatedly practised simulated tracheal access on a plastic larynx (Cricotrainer “FROVA”, VBM Medizintechnik GmbH, Sulz, Germany) until sufficiently confident to be tested.
Testing
Participants were tested on eFONA using both the Cric-Guide® device and the SBT technique. Each technique was repeated 4 times. Each participant was first tested using the Cric-Guide® and then the SBT technique. Given the obese model, the Cric-Guide® technique consisted of a vertical 8–10 cm scalpel incision followed by use of the red Cric-Guide® introducer, a 14 Fr bougie and a size 5.0 cuffed ETT, which is included in the Cric-Guide® packaging. They were then instructed to perform eFONA as per the recommended technique outlined by DAS (1) using a size 10 scalpel blade, a 14 Fr gum-elastic bougie and a size 6.0 ETT. Our primary outcome was the time taken from first handling of the equipment to successful inflation of the ETT cuff within the lumen of the trachea. Successful intubation of the trachea was confirmed by direct visual inspection of the open-ended distal tracheal lumen by the study team. Secondary outcomes included: the number of attempts taken to successfully insert the ETT into the trachea; the number of false passages created; the degree of posterior tracheal wall damage from photographs; the ease of penetrating the skin with the Cric-Guide® introducer and overall ease of use. The latter two used 10-point Likert scales (1= easy, 10= hard). False passage was defined as any passage of the bougie or ETT into the tissues or potential spaces surrounding the tracheal lumen.
Posterior tracheal wall trauma was assessed by a Consultant Head & Neck [Ear Nose & Throat (ENT)] surgeon. Each laryngo-trachea was split longitudinally through its anterior aspect and photographed. The surgeon graded the damage displayed in the photographs according to the following scale: 0, none; 1, mild (partial thickness laceration <5 mm); 2, moderate (>5 mm puncture/laceration); and 3, full thickness perforation (7). To demonstrate any damage in photographs a blue-gloved finger was placed behind any areas of interest to determine the depth of the injury. They were blinded as to the device used.
Statistical analysis
The distribution of data was assessed using the D’Agostino and Shapiro-Wilk tests. Given the repeated, dependent nature of the data, we used the Wilcoxon test to compare devices. The number of attempts, number of false passages and number of traumatic posterior wall lesions were expressed as median [interquartile range (IQR); range] and median of the differences [95% confidence interval (CI)]. Categorisation of severity of trauma used χ2 (Graph Pad Prism 9, San Diego, CA, USA) or Fisher’s test as appropriate. Spearman’s correlation (rho) was used to calculate the association between the number of attempts and procedure duration. In order to calculate the relative variance of independent variables on the primary outcome, we used generalizability theory (packages gtheory and lme4, Rstudio 2021.09.0, Boston, MA, USA). Trellis plots were created using ggplot2, Rstudio 2021.09.0, Boston, MA. We assumed that performance would be quicker with successive trials using the same device and follow a “learning curve” (8). The learning curve follows the power law. Therefore, in order to aid interpretation of graphs, we logged both the procedure (1, 2, 3 or 4) on the x-axis and the duration taken to complete the test on the y-axis. This enabled us to plot a straight best fit line through data. From this we calculated the slope of the line and the error around the slope (Figure 3).

Power calculation and sample size
Using repeated analysis [G*3 Power Dusseldorf (9)], and assuming an standard deviation (SD) of 68 s (10); estimated difference of 30 s between techniques; effect size of 0.44; a=0.05 and b=0.80, we needed to recruit 12 participants performing 4 paired procedures each, giving 96 procedures.
Results
Six consultant anaesthetists and six senior registrars in years ST6 and ST7, took part in the study. Six participants (consultants 6, registrars 6) had undertaken eFONA training in the SBT technique in the previous 6 months. No participant had any clinical experience of eFONA. All participants felt comfortable to proceed with the study after <10 min practice on the FROVA simulator.
In total, 96 procedures were performed, distributed equally between devices.
Study characteristics are given in Table 1. Time to secure the airway was less using the Cric-Guide® [median of differences 13 s (95% CI: 4 to 29), P=0.047], but was associated with greater trauma [median of differences 0 (95% CI: −1 to 0), P=0.008]. There were no instances in which the trachea was not eventually successfully intubated and the rates of false passage were not statistically different between techniques.
Table 1
| Outcome domain | Cric-Guide® (n=48) | Scalpel-bougie-tube (n=48) | Median of differences (95% CI) or RR (95% CI) | P value |
|---|---|---|---|---|
| Insertion time (s), median (IQR; range) | 58 (42–81; 23–251) | 72 (57–104; 30–235) | 13 (4 to 29) | 0.047 |
| Cricothyroid membrane identified (yes/no), n | 41/7 | 44/4 | 0.57 (0.19 to 1.71) | 0.52 |
| Attempts, n | 0 (0 to 0) | |||
| 1 | 30 | 29 | 0.292 | |
| 2 | 12 | 7 | 0.180 | |
| 3 | 4 | 6 | ||
| ≥4 | 2 | 6 | ||
| Median (IQR; range) | 1 (1–2; 2–4) | 1 (1–3; 1–6) | ||
| False passage, n | 0 (0 to 0) | |||
| 1 | 35 | 33 | ||
| 2 | 8 | 4 | 0.298 | |
| 3 | 3 | 6 | 0.159 | |
| ≥4 | 2 | 5 | ||
| Median (IQR; range) | 0 (0–1; 0–3) | 0 (0–1; 0–5) | ||
| Trauma, n | 0 (−1 to 0) | |||
| 0 | 18 | 28 | 0.042 | |
| 1 | 10 | 11 | 0.008 | |
| 2 | 16 | 9 | ||
| ≥3 | 4 | 0 | ||
| Median (IQR; range) | 1 (0–2; 0–3) | 1 (0–1; 0–2) | ||
| Ease of use† (Cric-Guide® only), median (IQR; range) | 3 (2–3; 1–8) | |||
| Future device preference, n | 11 | 1 | ||
| Learning slope, mean (SD) | −0.07 (0.20) | −0.08 (0.13) | −0.01 (−0.20 to 0.17) | 0.88 |
†, 1–10, easy to hard. CI, confidence interval; RR, relative risk; IQR, interquartile range; SD, standard deviation.
In cases where the CTM was successfully identified it was used as the point of entry into the trachea. Where this was not the case, entry was via direct entry between tracheal rings.
The correlation between number of attempts and time to complete the procedure was 0.67 (95% CI: 0.48–0.81, P<0.001) using the Cric-Guide® and 0.71 (95% CI: 0.52–0.83, P<0.001) using the SBT.
Participant feedback revealed that on a ten-point Likert scale from 1–10 (1= easy and 10= hard) the average score for the Cric-Guide® was 2.9 and the median score was 3. The minimum score was 1 and the maximum 8. Five participants reported that the Cric-Guide® was ‘easy’ to insert through the skin and seven ‘moderate’.
Generalizability statistics showed that the majority of variance of a statistical model predicting successful outcome was attributed to the number of attempts (74%), residual error (16%), subjects (7%), and type of device (1%).
Discussion
In this study, participants secured eFONA quicker using the Cric-Guide® compared to the SBT technique. More rapid airway control came at the expense of greater posterior tracheal wall trauma. Across the remaining outcome measures (number of attempts required and creation of a false passage) the Cric-Guide® was shown to be non-inferior to SBT.
Chauhan and colleagues (11) performed a similar study in a benchtop model comparing Cric-Guide® and SBT in both slim and obese necks. In contrast to our study, they failed to show that Cric-Guide® resulted in faster access to the airway in the obese neck, however, they did not demonstrate increased rates of trauma. Their technique was, however, different to ours in that they did not carry out a DAS recommended 8–10 cm incision in the obese neck and relied on identification of the midline by palpation. Their model did not include blood. This variation of the technique and the omission of blood may explain the lower rate of trauma but also the lack of time difference.
Dannatt and colleagues (12) tested the Cric-Guide® in a slim and bleeding neck model and similarly to our work showed that there was an increased rate of posterior laryngeal wall damage but that there was no time difference when compared with SBT.
In light of this work, our study both corroborates previously published data but demonstrates that with a modified technique, more rapid access to the airway can be achieved.
On the basis of our finding of increased tracheal trauma with the red introducer in the obese model, we propose a modified technique to that recommended by the manufacturer to reduce the incidence and severity of posterior tracheal wall damage when Cric-Guide® use follows a vertical incision in the impalpable neck. The manufacturer suggests using a ‘Red’ size device (30 mm blade length) in the obese patient and stabilising its wings on the operator’s index finger to limit depth of insertion (6). However, we observed that once the midline incision was performed the tissues splayed laterally and operators were reluctant to have fingers in the way of the device. Our proposed modification would be to utilise a shorter device designed for slimmer patients. It is proposed that this would be long enough to reach and enter the trachea after a vertical incision but reduce incidence of trauma to the trachea. This modification requires further research—as highlighted by both Chauhan (11) and Dannatt (12).
Wide variability is demonstrated between operators with some demonstrating high degrees of proficiency throughout, and others steep, learning curves. This reflects the reality that depending on the individual operator, patient, situation, and stress associated with a given situation—performance will vary.
Participant feedback was positive regarding the Cric-Guide® device and the realism of the simulation model. Eleven participants would choose to use the Cric-Guide® device in future eFONA procedures over the SBT technique. Participants indicated that they felt the tissue model accurately simulated the clinical scenario desired and that they would wish to practice on it more in the future. They also were clear that preforming either technique was much more challenging than they had anticipated and that they had a new-found respect for the ‘difficult front of neck access’ situation. Anaesthetists are not trained to make large incisions, nor manage blood filling the wound. We suggest simulating this scenario on a regular basis to familiarise them with this technique.
Our model was relatively inexpensive to create and the materials required were straightforward to source. Furthermore, it created an acceptably close representation of the required anatomy and tissue behaviour required for accurate simulation. We propose that practicing for ‘difficult front of neck access’ should become routine and offer our model as a means to achieve this in local departments.
Conclusions
In conclusion, the Cric-Guide® performed better than the SBT technique in the time taken to secure FONA in the simulated obese neck with blood, however, it was non-inferior in number of attempts taken and false passage creation. Further research is needed to determine whether reduced rates of posterior laryngeal wall trauma can be achieved by using a different sized Cric-Guide® device. Given the more rapid performance of participants using the Cric-Guide® and its preference to operators, we believe that it will be a useful tool in the performance of eFONA moving forward.
Acknowledgments
Presentation: Preliminary data was presented as a poster at the Difficult Airway Society Annual Scientific Meeting Newcastle, UK, 2022.
Assistance with this article: Dr. Richard Vanner (inventor of Cric-Guide®) provided the devices, the endo-tracheal tubes and gum-elastic-bougies used in this study. Dr. Vanner had no input into the conduct of the study or the drafting of the manuscript.
Funding: We are grateful to
Footnote
Data Sharing Statement: Available at https://joma.amegroups.com/article/view/10.21037/joma-23-16/dss
Peer Review File: Available at https://joma.amegroups.com/article/view/10.21037/joma-23-16/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://joma.amegroups.com/article/view/10.21037/joma-23-16/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was reviewed by the Clinical Governance Department of Tayside Health Board and deemed not to require ethical review (on April 21, project registration number 017/21). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All participants gave their consent to participate in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015;115:827-48. [Crossref] [PubMed]
- Lowes T. 'Bougie-assisted' cricothyroidotomy technique. Br J Anaesth 2016;117:540-1. [Crossref] [PubMed]
- Yeow C, Greaney L, Foy C, et al. Evaluation of a novel cricothyroidotomy introducer in a simulated obese porcine model: a randomised crossover comparison with scalpel cricothyroidotomy. Anaesthesia 2018;73:1235-43. [Crossref] [PubMed]
- Gadd K, Wills K, Harle R, et al. Relationship between severe obesity and depth to the cricothyroid membrane in third-trimester non-labouring parturients: a prospective observational study. Br J Anaesth 2018;120:1033-9. [Crossref] [PubMed]
- Vanner R. Cric Guide. 2018. Available online: https://www.youtube.com/watch?v=SNn54YV9XW4
- Vanner R. Cric-Guide cricothyrotomy with impalpable CTM. 2019. Available online: https://www.youtube.com/watch?v=ZjMDhHoORTQ
- Maini N, Crawley SM. A pilot study of a novel cricothyroidotomy device in Thiel cadaveric models. Eur J Anaesthesiol 2021;38:316-7. [Crossref] [PubMed]
- McLeod G, McKendrick M, Tafili T, et al. Patterns of Skills Acquisition in Anesthesiologists During Simulated Interscalene Block Training on a Soft Embalmed Thiel Cadaver: Cohort Study. JMIR Med Educ 2022;8:e32840. [Crossref] [PubMed]
- Erdfelder, Faul, Buchner. G*3 Power, Dusseldorf. 1996. Available online: https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower
- Le Fevre PJ, Gough C, Hearne BJ, et al. A trial comparing emergency front of neck airway performance in a novel obese-synthetic neck, meat-modified obese neck and conventional slim manikin. Anaesthesia 2019;74:480-7. [Crossref] [PubMed]
- Chauhan SK, Monaghan M, McCaul CL. Evaluation of a novel emergency front of neck access device in a benchtop model of obesity. Ir J Med Sci 2022;191:413-20. [Crossref] [PubMed]
- Dannatt PJ, Choo YY, Barron A, et al. Comparing the Cric-Guide® emergency front of neck access device to a scalpel-bougie-tube technique in a porcine model that simulates bleeding: A randomised crossover study. Eur J Anaesthesiol 2022;1:e008.
Cite this article as: Belford I, Wright K, Janeczko A, Crawley S, McLeod G, Maini N. A comparison of scalpel-bougie-tube and Cric-Guide® in a simulated obese bleeding tissue model. J Oral Maxillofac Anesth 2023;2:23.



