
Extravasation of irrigant to the parapharyngeal space during temporomandibular joint (TMJ) arthroscopy requiring prolonged intubation: a case report and review of the literature
Introduction
Temporomandibular joint (TMJ) arthroscopy is a common modality for the diagnosis and treatment of temporomandibular joint disease (TMD). It was first described in 1975 by Onishi (1). The technique of TMJ arthroscopy for diagnosis and treatment of TMD was further described in 1988 by McCain in a study of 67 cadaveric joints (2).
The procedure of TMJ arthroscopy primarily involves the superior joint space. It is first insufflated, then a sharp trocar is used to introduce the cannula that houses the arthroscope. An additional operative cannula can be inserted for advanced arthroscopy (3). An external view of the set-up for TMJ arthroscopy is displayed in Figure 1.

Complications of TMJ arthroscopy are generally uncommon. McCain and González-García et al. reported complication rates of 1.34–4.4% (4,5). The known complications of TMJ arthroscopy include: facial palsy (from damage to the facial nerve, most commonly the frontal branch), hearing loss (from damage of the eighth cranial nerve, tympanic disruption, and ossicle disruption with entry in the middle ear, otitis media, and hypoacusia), perforation of the glenoid fossa, hemarthrosis, infection, and damage to the articular disc (6). This case report describes the observation and management of extravasation of irrigant causing delayed extubation, an uncommon complication of TMJ arthroscopy. We present the following cases in accordance with the CARE reporting checklist (available at https://joma.amegroups.com/article/view/10.21037/joma-21-16/rc). This manuscript adheres to the applicable EQUATOR guideline and written HIPAA authorization was obtained.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Patient #1
A 19-year-old female presented with jaw pain, TMJ clicking and multiple instances of a closed lock (limited mouth opening from TMJ disc abnormality), which failed conservative management (NSAIDs, orthotic, and physical therapy). MRI of the TMJ revealed anterior displacement of the meniscus of the left TMJ and a right sided synovial cyst. Computed tomography was negative for erosive changes of the condylar heads bilaterally. Given her history and radiographic findings, she was a candidate for bilateral TMJ arthroscopy
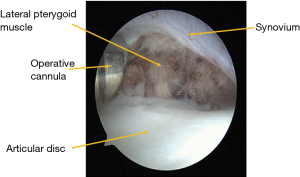
On the day of the procedure, the patient was intubated with asleep fiberoptic nasotracheal intubation with a cuffed 6.0 nasal RAE endotracheal tube, which was sutured to the nasal septum. The left TMJ was operated first. A patent irrigation system of the joint was established and the arthroscope was inserted into the superior joint space. A biopsy of the anteromedial synovium was performed followed by myomotomy of the lateral pterygoid muscle attachment to the anteromedially displaced disc in preparation of disc repositioning (Figure 2). During posterior repositioning of the disc, swelling of the temporal and parotid regions, and excessive jaw stiffness were identified by the surgical team (Figure 3). The right TMJ was then operated on with a similar entrance as the left side. After completion of the right TMJ treatment, a significant amount of left sided facial edema remained. Direct laryngoscopy was performed, and it was found that there was severe swelling of the left parapharyngeal space as well as the soft palate (Figure 4). Given this airway edema, it was determined to keep the patient intubated with the existing endotracheal tube. She was transported to the intensive care unit and remained intubated overnight. On post-operative day 1, approximately 15.5 hours after the end of surgery, the patient was evaluated clinically and deemed safe for extubation and was extubated without issue. On examination, there was only minimal amounts of swelling of the palate and left parapharyngeal space. She was monitored for 1 more day and was discharged on postoperative day 2.

Patient #2
A 63-year-old female presented with right sided facial pain and was found to have ankylosis of the right TMJ. CT imaging revealed heterotopic bone over the right condyle fossa complex. MRI revealed degenerative changes of the right TMJ with an anteriorly displaced articular disc. The recommended definitive treatment was total joint replacement. Prior to the planned procedure, the patient developed induration and erythema over the right TMJ region. Diagnostic TMJ arthroscopy was performed for a concern of septic arthritis.
On the day of the procedure, an asleep fiberoptic nasotracheal intubation was performed with a cuffed 6.5 nasal RAE sutured to the nasal septum. The arthroscope was inserted into the superior joint space of the right TMJ with findings of an ankylotic joint with fibrotic tissue and no purulence. Biopsies of tissue were taken, and joint lavage was performed. Facial swelling developed and direct laryngoscopy reveled edema of the right parapharyngeal space. Given the airway edema, the patient was transported to the post-anesthesia care unit where video laryngoscopy was performed and revealed right parapharyngeal swelling without glottic edema. She was then kept intubated for 24 hours and extubated without issue on post-operative day 1.
Discussion
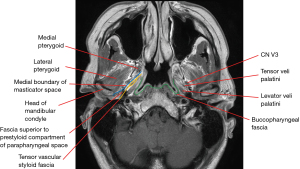
Extravasation of irrigant to the parapharyngeal space during TMJ arthroscopy has been previously discussed in the literature (7). The parapharyngeal space (also known as the lateral pharyngeal space) is a space that lies on either side of the neck and is composed of a prestyloid and retrostyloid component. The borders the parapharyngeal space are variable throughout the literature, but the following boundaries have been proposed. The medial wall of the parapharyngeal space is formed by the buccopharyngeal fascia (BPF) as it covers the outer aspect of the pharyngeal constrictors (8). The lateral border is marked by the medial pterygoid muscle along with the fascial layer extending from the muscle to the skull base (9). Anteriorly the BPF and the interpterygoid fascia fuse at the pterygomandibular raphe. This space extends from the skull base superiorly to the angle of the mandible inferiorly. The posterior border is thought to consist of the carotid sheath in the retrostyloid compartment of the parapharyngeal space. The parapharyngeal space is described as communicating with the submandibular space inferiorly (10). This could explain sublingual and submandibular swelling that can also be seen with extravasation.
Based on this anatomy, is hypothesized by the authors that the fluid will extravasate along the superior belly of the lateral pterygoid muscle within the masticator space. Then, by an unclear mechanism, the irrigant exits the masticator space and travels along the tensor vascular styloid fascia within the prestyloid compartment parapharyngeal space where it can also communicate with the sublingual and submandibular spaces (Figure 5).
One study by Sasaki et al. attempted to elucidate the mechanism of extravasation and injected contrast medium into 43 joints and found extravasation of contrast medium with 9 of the joints, most commonly occurring at the anteromedial aspect (11). TMJ arthroscopy was completed on 2 of these 9 joints and no perforation was identified surgically. Anatomically it is known that, especially during pathological states, the pterygoid shadow at the anteromedial aspect of the joint space can become thin to the point a perforation may be seen resulting in herniation of the lateral pterygoid muscle into the superior joint space (12).
Other causes of extravasation of fluid include iatrogenic perforation of the medial joint space during insufflation. This can occasionally be identified by lack of plunger rebound after the insufflation of the superior joint space with 2–3 cc of fluid. It is also possible that increased irrigation pressure could also increase the amount of fluid that extravasates. It is important that the irrigation system remains patent and that the surgical team monitor the patency of this system.
During the surgery, this patient initially presented with external facial swelling which prompted further investigation of the airway by the surgical and anesthesia teams. Often this is also associated with a decreased mobility of the joint. The two cases reported suggest that involvement of the parapharyngeal space and delayed extubation should be considered a known complication of TMJ arthroscopy. Our experience reveals rapid resolution of the swelling. Some case reports have described successful extubation after one to two hours post operatively (7,13,14). Physical exam (not limited to intraoral exam of pharyngeal tissues, the use of video laryngoscopy, or nasopharyngoscopy) and assessment of clinical criteria are essential for determining timing of extubation. The resolution of the extravasation of this sterile irrigant should not be compared to that of an inflammatory process, as in the former case, resolution can be quite rapid and frequent assessments should be performed to ensure that the patient can be extubated in a timely fashion. The authors have chosen to highlight this case report as it is important for both the surgical and anesthesia teams to recognize and properly manage this potential airway complication of TMJ arthroscopy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://joma.amegroups.com/article/view/10.21037/joma-21-16/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://joma.amegroups.com/article/view/10.21037/joma-21-16/coif). JPC serves as an unpaid editorial board member of Journal of Oral and Maxillofacial Anesthesia from July 2021 to June 2023. JW serves as an unpaid editorial board member of Journal of Oral and Maxillofacial Anesthesia from August 2021 to July 2023. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Onishi M. Arthroscopy of the temporomandibular joint. Kokubyo Gakkai Zasshi 1975;42:207-13. [Crossref] [PubMed]
- McCain JP. Arthroscopy of the human temporomandibular joint. J Oral Maxillofac Surg 1988;46:648-55. [Crossref] [PubMed]
- McCain JP, Hossameldin RH. Advanced arthroscopy of the temporomandibular joint. Atlas Oral Maxillofac Surg Clin North Am 2011;19:145-67. [Crossref] [PubMed]
- González-García R, Rodríguez-Campo FJ, Escorial-Hernández V, et al. Complications of temporomandibular joint arthroscopy: a retrospective analytic study of 670 arthroscopic procedures. J Oral Maxillofac Surg 2006;64:1587-91. [Crossref] [PubMed]
- McCain JP, Sanders B, Koslin MG, et al. Temporomandibular joint arthroscopy: a 6-year multicenter retrospective study of 4,831 joints. J Oral Maxillofac Surg 1992;50:926-30. [Crossref] [PubMed]
Advanced Arthroscopy of the Temporomandibular Joint- ClinicalKey - Kassam K, Cheong R, Cascarini L. Parapharangeal edema: an uncommon complication of TMJ arthroscopy. Clin Case Rep 2015;3:496-8. [Crossref] [PubMed]
- Som PM, Curtin HD. Fascia and spaces of the neck. In: head and neck imaging. 5th ed. Philadelphia (PA): Mosby, 2011:2203-34. Available online: https://www-clinicalkey-com.ezp-prod1.hul.harvard.edu/#!/content/book/3-s2.0-B9780323053556000367
- Curtin HD. Separation of the masticator space from the parapharyngeal space. Radiology 1987;163:195-204. [Crossref] [PubMed]
- Grodinsky M, Holyoke EA. The fasciae and fascial spaces of the head, neck and adjacent regions. Am J Anat. 1938;63:367-408. [Crossref]
- Sasaki K, Watahiki R, Tamura H, et al. Fluid extravasation of the articular capsule as a complication of temporomandibular joint pumping and perfusion. Bull Tokyo Dent Coll 2002;43:237-42. [Crossref] [PubMed]
- McCain JP. Principles and practice of temporomandibular joint arthroscopy. 1st edition. Philadelphia (PA): Mosby, 1996.
- Carls FR, Engelke W, Locher MC, et al. Complications following arthroscopy of the temporomandibular joint: analysis covering a 10-year period (451 arthroscopies). J Craniomaxillofac Surg 1996;24:12-5. [Crossref] [PubMed]
- Fernández Sanromán J, Costas López A, Fernández Ferro M, et al. Complications of temporomandibular joint arthroscopy using two-portal coblation technologies: A prospective study of 475 procedures. J Craniomaxillofac Surg 2016;44:1221-5. [Crossref] [PubMed]
Cite this article as: Zacharias JR, McCain JP, Curtin HD, Wang J, Hakim MA. Extravasation of irrigant to the parapharyngeal space during temporomandibular joint (TMJ) arthroscopy requiring prolonged intubation: a case report and review of the literature. J Oral Maxillofac Anesth 2022;1:8.



